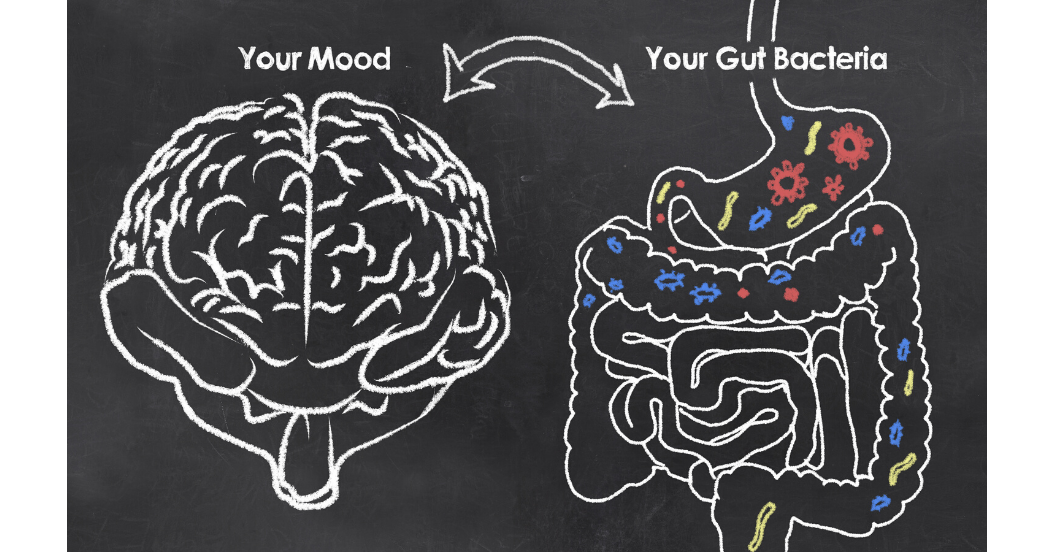
 There is a large relationship between mental health problems and digestive disorders. For example, anxiety is five times higher in individuals with irritable bowel syndrome (IBS) than in those with no IBS symptoms, and among anxiety sufferers, rates of IBS (and other functional gastrointestinal disorders) are increased fourfold. Research has shown that it is common that a diagnosis of anxiety or depression will precede a diagnosis of IBS by approximately 3.5 years, and experimental studies have shown that psychosocial stress can increase IBS symptoms. The opposite direction has also strong support showing that digestive disorders can precede and cause mood disorders.
There is a large relationship between mental health problems and digestive disorders. For example, anxiety is five times higher in individuals with irritable bowel syndrome (IBS) than in those with no IBS symptoms, and among anxiety sufferers, rates of IBS (and other functional gastrointestinal disorders) are increased fourfold. Research has shown that it is common that a diagnosis of anxiety or depression will precede a diagnosis of IBS by approximately 3.5 years, and experimental studies have shown that psychosocial stress can increase IBS symptoms. The opposite direction has also strong support showing that digestive disorders can precede and cause mood disorders.
Research has consistently shown that exposure to early life adversity is a potent risk factor for both GI and mental illnesses. Rats exposed to parental-deprivation stress exhibit increased IBS symptoms (i.e., visceral hypersensitivity) as well as elevated levels of anxiety at postweaning age, and into adulthood, compared to nondeprived peers. In humans, early adversity (particularly in the late postnatal period) is associated with up to a threefold increase in risk of irritable bowel symptoms and contributes to over a third of lifetime mental illness diagnoses, as well as subthreshold and clinical levels of anxiety in children.
Early adversities in life have been shown to alter brain structures such as the prefrontal cortex, amygdala, and hippocampus. Changes in these brain structures may cause changes in cognition, mood and emotional regulation, as well as lead to mood disorders and chronic pain syndromes. Early adversities and mood disorders have also been associated with altered microbiomes (gut bacteria), especially if the trauma occurs during key developmental periods. The fact that early experiences of caregiving adversity increase the risk for both GI and mental health problems, as well as being associated with changes to the GI microbiome, suggests that the timing of this exposure (infancy to early childhood) coincides with the sensitive period for the maturation of each of these systems.
This further highlights the importance of mind-body forms of medicine. The combination of a nurturing environment combined with a healthy diet and exercise continues to show support in research as an optimal scenario for both children and adults.
Reference
Mind and gut: Associations between mood and gastrointestinal distress in children exposed to adversity. Development and Psychopathology. 2019.